The Food and Drug Administration (FDA) has cleared the clinical use of two biomedical imaging technologies developed with support from the National Institute of Biomedical Imaging and Bioengineering (NIBIB). Both technologies offer advances in computed tomography (CT).
In one of these developments, project leader Cynthia McCollough, Ph.D., director of Mayo Clinic’s CT Clinical Innovation Center, and her team helped develop the first photon-counting detector (PCD) CT system, which is superior to current CT technology. Computed tomography has been an immense clinical asset in diagnosing many diseases and injuries. However, since its introduction into the clinic in 1971, the way the CT detector converts x-rays into electrical signals has remained essentially the same. Photon counting detectors operate using a fundamentally different mechanism than any previous CT detector.
“This is the first major imaging advance approved by the FDA for CT in a decade,” said Behrouz Shabestari, Ph.D., director of the Health Informatics Technologies division. “The impact of this development will be far-reaching and will provide doctors with more detailed information for medical diagnoses.”
A CT scan is obtained when an x-ray beam rotates around a patient, allowing the x-rays to pass through the patient. As the x-rays leave the patient, a detector takes a photograph and the information is transmitted to a computer for further processing. “Standard CT detectors use a two-step process, in which X-rays are converted to light and then the light is converted to an electrical signal,” explained Cynthia McCollough. “The photon counting detector uses a single-step process in which X-rays are immediately transformed into an electrical signal.”
In the two-step CT process, the energy of the X-rays is not recorded, but in the single-step process, individual X-rays are recorded along with their energy level. As the x-rays rapidly enter the detector, they are counted (hence the name photon counting) and classified according to their energy. Based on physical principles, this helps identify different materials (e.g., iodinated blood, soft tissues, bones) more easily.
This specific type of image is called multi-energy CT. “Dual-energy CT requires specialized equipment and is limited to two energies, but with this new detector we have more ‘buckets’ to sort through X-ray energies and that gives us the opportunity to better represent the differences between materials.” McCollough described.
In clinical studies published in Radiology, noise reduction of up to 47 percent was achieved with new PCD-CT systems1. “Noise” refers to the random nature of X-ray signals, which makes images more difficult to interpret due to the associated speckle pattern that is superimposed on the true image structures.
The new system also reduces the amount of contrast agent needed for CT imaging. CT scan is effective in visualizing blood vessels and tumors, but contrast agents must be used to achieve this. Contrast agents are safe for most patients, but in certain cases it may be better to give a lower dose, if possible. Because there is more contrast agent signal with the PCD-CT system, study participants needed thirty percent less contrast agent to achieve the same image quality as with conventional CT systems.2.
PCD-CT systems also have better spatial resolution compared to conventional systems. In studies, the system achieved the best resolution reported for a clinical CT system2. McCollough compared it to a digital camera: the higher the number of megapixels, the more detail you can see. “The significantly improved resolution and increased signal are the innovative advantages this CT system has over standard CT,” Shabestari said.
McCollough and his team at Mayo Clinic in Rochester, Minnesota, have been working on this project with Siemens Healthineers in Forchheim, Germany, and Siemens Medical Solutions in Malvern, Pennsylvania, for the past 10 years. Siemens had been working on a prototype PCD-CT system and with McCollough NIBIB funding The team was able to begin scanning patients with approval from the Institutional Review Board. In these studies, more than 1,100 patients have been scanned, first with a conventional CT system and then with the new PCD-CT scanner, to show the advantages of the new system. The device is the first of its kind on the market.
McCollough is also trying to find other ways to improve CT for doctors using artificial intelligence (AI). His group is applying deep learning (DL) methods to reduce noise (and radiation dose) without altering image anatomy. He noted: “You can see more with AI processing – it makes a big difference.”
Using AI to develop software to improve brain scans
NIBIB-funded researcher Danny JJ Wang, PhD, director of imaging technology innovation at the Mark and Mary Stevens Institute for Computing and Neuroimaging at the University of Southern California, and his team at startup Hura Imaging, Inc. have also been using AI to reduce the radiation dose administered to a patient when undergoing a conventional CT scan.
Although CT imaging is very safe, patients are exposed to small doses of radiation. Patients who need repeat scans to monitor their health or a specialized CT exam, CT perfusion (CTP), are exposed to higher doses of radiation. Radiologists must balance the use of lower dose CT scans, which produce lower quality images, with the use of higher doses to obtain better quality images for making diagnostic and treatment decisions.
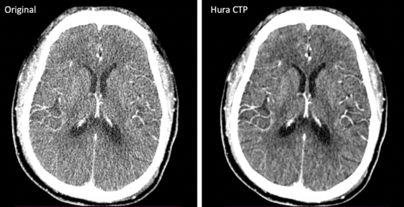
CTP is used to evaluate damage to the brain in a patient with suspected stroke. To reduce the high radiation dose in CTP, Wang and his colleagues turned to AI and developed software to assist in image reconstruction. The software uses an algorithm called K-Space Weighted Image Averaging that reduces noise from CTP images and subsequently reduces the radiation dose delivered to the patient without compromising image quality or processing speed.
Studies showed that the software reduces CTP radiation dose by 50% to 75% compared to standard CTP methods.4. Other advantages of using the method include no disruption to standard clinical workflow and no upgrades or modifications to current CT hardware. The software has received 510(k) clearance from the FDA and can be adopted into clinical practice. “Currently, this is only applicable to time-series CT data such as CT perfusion and dynamic CT angiography, but we are developing deep learning-based algorithms so that in the future the software can be applied to all forms of CT imaging,” Wang said.
Wang received his second Small Business Innovation Research Award of NIBIB to develop the software from use in the laboratory to commercialization for broader impact. “This is an excellent example of a NIBIB-supported technology that has resulted in an FDA-approved product and can be used in clinical practice,” said Qi Duan Ph.D., program director in Image Processing, Visual Perception and Visualization.
1Rajendran K, Petersilka M, Henning A, Shanblatt E, Marsh J Jr, Thorne J, Schmidt B, Flohr T, Fletcher J, McCollough C, Leng S. Full-field-of-view, high-resolution photon-counting detector CT: technical evaluation and initial patient experience. 2021 Oct 27;66(20):10.1088/1361-6560/ac155e. doi:10.1088/1361-6560/ac155e. PMID: 34271558; PMCID: PMC8551012.
2Kishore Rajendran, Martin Petersilka, André Henning, Elisabeth R. Shanblatt, Bernhard Schmidt, Thomas G. Flohr, Andrea Ferrero, Francis Baffour, Felix E. Diehn, Lifeng Yu, Prabhakar Rajiah, Joel G. Fletcher, Shuai Leng and Cynthia H. McCollough First clinical CT system with photon counting detector: technical evaluation Radiology 2022 303:1, 130-138.
3Benson JC, Rajendran K, Lane JI, Diehn FE, Weber NM, Thorne JE, Larson NB, Fletcher JG, McCollough CH, Leng S. A new frontier in temporal bone imaging: photon-counting detector CT demonstrates superior visualization of critical anatomical structures with reduced radiation dose. AJNR Am J Neuroradiol. 2022 April;43(4):579-584. doi: 10.3174/ajnr.A7452. Epub dated March 24, 2022. PMID: 35332019; PMCID: PMC8993187.
4Zhao C, Martin T, Shao X, Alger JR, Duddalwar V, Wang DJJ. Low-dose CT perfusion with K-space weighted image averaging (KWIA). IEEE Trans Med Images 2020 Dec;39(12):3879-3890. doi: 10.1109/TMI.2020.3006461. Epub 30 Nov 2020. PMID: 32746131; PMCID: PMC7704693.