The next frontier of medicine will not be defined by a single technology or treatment. It will be defined by how primary care is practiced.
Today’s physicians are asked to keep pace with accelerating science while managing increasing patient demands and systemic inefficiencies, leaving even the most dedicated on the edge. The answer is not to expect more from them. It is about changing the model, creating partnerships that provide advanced science, data and proactive strategies for the interception of diseases directly together with primary care.
In this emerging approach, physicians are no longer isolated but supported by collaborators who amplify their reach and help patients maintain the quality of their lives. That future is closer than many believe and may radically redefine what it means to practice medicine.
Innovation in healthcare has never advanced so quickly. Advances in genomics, imaging and machine learning are expanding the possibilities for earlier detection, targeted interception and more personalized treatment. However, the gap between discovery and adoption in primary care remains wide. Doctors simply do not have the time or infrastructure to evaluate every new diagnostic paper, device or tool, and patients often wait years before life-changing innovations reach daily practice. That delay comes at a cost: missed opportunities to intercept the disease before it progresses and optimize patients’ health when it matters most.
Closing this gap requires a new type of partnership. Remaining at the center of trusted, patient-centered relationships, independent physicians can expand their impact by working with partners who specialize in examining, integrating and applying the latest advances. Instead of taking on the impossible task of staying up-to-date in all fields of medicine, primary care physicians can take advantage of a collaborative ecosystem that provides them with real-time insights, curated evidence, and clear guidance on what is clinically feasible for their patients.
While it is up to them to determine the best treatment plan for their patients, primary care doctors can only recommend what they know. Advances are rapidly transforming the healthcare landscape, but it is nearly impossible for physicians to sort through the available information to integrate these techniques into their patient care regimens. What is needed is a way for physicians to increase their ability to learn and effectively use cutting-edge technologies and diagnostics to provide better patient care while fostering practice growth.
An ER doctor I knew who worked in concierge primary care approached me a few years ago. She knew I had been in the precision genomic medicine space and wanted a partner who could inform her and help her integrate cutting-edge science into her practice. He is confident in his abilities, but acknowledged that genomics was not part of his training. He wanted to help his patients and quickly grow his practice’s capabilities, and saw the partnership as a viable way to do so quickly.
This desire for expert partners is not surprising; There is a considerable amount of research out there, but with the sheer number of appointments they have to make (seeing patients every 15 to 30 minutes), doctors are hard-pressed to find the bandwidth to dive into it. An increasing number of primary care physicians often want to be part of larger institutions because they can gain access to key opinion leaders and learning components that are pre-vetted and shared with them. It is efficient, saves time and effort, and provides real value in terms of being able to apply the latest science and being the first in your markets to share these benefits with your patients.
But independent primary care physicians can also benefit from partners who can advance their capabilities by leading with science that has clinical applicability and is useful to their patients and their communities. That means promoting early disease detection, advanced diagnosis and interception. They seek information and technology that helps them practice medicine in the best way possible.
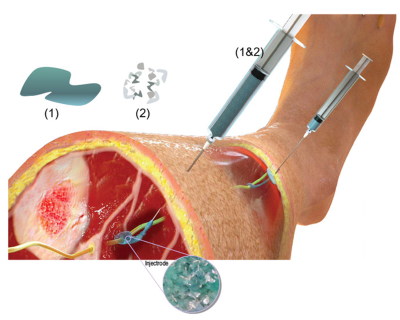
Three key components that have historically been out of reach for many in primary care will be game-changers: genomics, proteomics, and imaging. While many analyze the images, each MRI machine is different and there are many natural anatomical variations or benign findings. How do you solve that? Clinicians should not rely on any technology to be universally applicable; These technologies must work together to paint a complete diagnostic picture.
Neurodegeneration is a good example. The newest technology focuses on proteomics; In May, the U.S. Food and Drug Administration (FDA) approved the Lumipulse G pTau217/ß-Amyloid 1-42 plasma test, the first blood-based diagnostic to aid in the detection of Alzheimer’s disease. But there are other factors that could elevate other proteomics, such as glial fibrillar proteins or neurofilaments. To better elucidate the clinical picture, aspects such as functional testing and neuroimaging should come into play to obtain the overall picture. For a primary care physician, it is nearly impossible to analyze all the research and data on which tools are most reliable or how they fit together, while managing entire panels of patients on a daily basis. But with expert partners, these technologies can be synthesized into a coherent picture, linking genomics, proteomics and imaging to track changes over time and give patients a clearer view of their future health trajectory.
If a doctor looks at any of the individual categories, it is very easy to get it wrong, but partnering with experts in the field allows them to examine a patient’s genomic pattern and predisposition. A partner employs equipment that can look at all three categories to see if there are anatomical volume changes in the major areas of the patient’s brain and can longitudinally record the changes that occur year after year. This is how a primary care doctor can access key information that tells them which direction their patient is going.
When you try to do everything, you don’t do anything well. This collaborative model can only work when it is seen (and sees itself) as a true subspecialty that makes diagnostic advances and technological solutions affordable and accessible to a large number of primary care physicians, a subspecialty that focuses on precision genomic medicine and doing it extremely well. This is not about overwhelming doctors with more information; It’s about giving them the right support at the right time, so they can focus on what’s most important: guiding patients through decisions that shape their quality of life.
The future of primary care will be collaborative by design. Doctors will still be the first call and trusted guide, but they will be supported by scientific partners who bridge the gap between breakthrough and bedside. Together, they can go from treating disease after it appears to intercepting it before it takes hold, helping patients live not only longer, but healthier.
Photo: PeopleImages, Getty Images
Dr. Julie Chen He is the medical director of radence. He previously held a similar role at Human Longevity and Vitagene. His research, conducted at the FDA, NIH, National Cancer Institute, USC, and Mount Sinai, has shaped scientific advancement in precision medicine. As a physician specializing in integrative internal medicine, she developed numerous corporate wellness programs in Silicon Valley focusing on a whole systems approach to healthcare. Dr. Chen frequently provides medical commentary for broadcast outlets such as ABC, NBC, FOX and MSN, and has appeared in national publications and podcasts. In 2023, Healthcare Technology Report named her among the top 25 women leaders in biotechnology for her leadership in the development of healthcare technologies. Dr. Chen is a member of the Buck Institute President’s Circle, dedicated to advancing research on aging and longevity.
This post appears through MedCity Influencers program. Anyone can post their perspective on business and healthcare innovation to MedCity News through MedCity Influencers. Click here to find out how.