Wearable ultrasound patches have the potential to revolutionize healthcare, facilitating remote monitoring of critical physiological functions in the comfort of the patient’s home. But most patches in development have a major limitation: They require cables to power the device and transmit ultrasound data, physically tethering the user to a control system. That is, until now.
A fully wireless ultrasound patch has been launched that can continuously track critical vital signs such as heart rate and blood pressure. recently reported in Nature Biotechnology. The patch, which can capture detailed medical information and transmit the data wirelessly to a smart device (such as a laptop or smartphone), could represent a big step forward in home healthcare technology.
“The true impact of wearable ultrasound patches has not yet been fully understood, as the iterations described above are not wireless and limit users’ ability to go about their daily lives,” said Randy King, Ph.D., program director in NIBIB’s Division of Applied Science and Technology. “The technology described here represents necessary and essential progress in the portable ultrasound space, potentially unlocking the promise of remote ultrasound monitoring for any number of health conditions.”
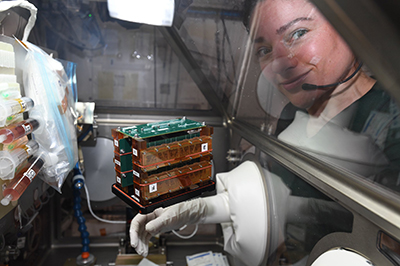
Ultrasound, which uses sound waves and their resulting echoes to image tissues within the body, has traditionally been limited to the clinic. The ultrasound patch technology in this study was pioneered by Sheng Xu, Ph.D., associate professor and Jacobs Faculty Scholar at the University of California, San Diego (UC San Diego). His team has previously reported on wearable ultrasound patches with similar transducers. The real breakthrough in this latest study is the wireless capability of the patch.
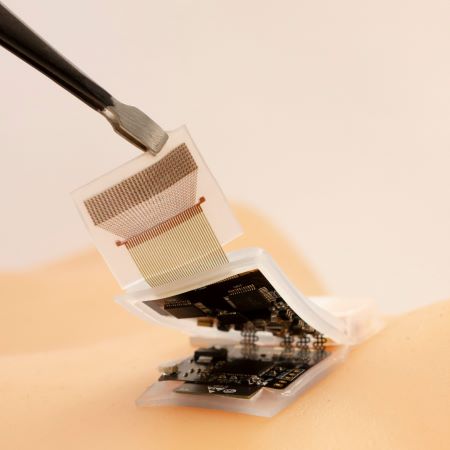
“The key element of this study is the design of the ultrasound circuit,” Xu said. “In our previous patches, the ultrasound probe was connected to a flexible cable for power and data transmission. In this patch, the cables are replaced with a wearable circuit, which can pre-process and wirelessly transmit the ultrasound data to a back-end station for further analysis.”
The ultrasound system is made up of a probe, a circuit and a battery. As the current system was designed with a focus on cardiovascular health, in this study the ultrasound probe was generally placed in the carotid artery. The probe is connected to a flexible circuit that activates the ultrasound transducers, collects the ultrasound echoes, amplifies and filters them, and transmits the digitized signal to a terminal device. The entire system is powered by a commercial rechargeable lithium polymer battery.
“We developed a machine learning algorithm to coordinate with the circuit to automatically process ultrasound signals and continuously track the carotid artery, allowing us to obtain ultrasound information even when the patch wearer is moving,” explained first author Muyang Lin, Ph.D. candidate in the Xu laboratory. “This automatic tracking algorithm offers unprecedented opportunities for medical ultrasound and exercise physiology.”
To evaluate its generalizability, the researchers cross-validated their machine learning model among ten healthy subjects representing three different racial groups. Using a machine learning technique called domain adaptation, the researchers found that a model trained with data from one participant wearing the patch could successfully adapt for the other participants. With minimal model retraining, the patch could track carotid artery pulsations with high precision, enabling measurements such as blood pressure, arterial stiffness, and cardiac output. Continued monitoring of these measurements among high-risk populations could provide an early warning of heart failure.
“Validating our patch in a larger population is the crucial next step,” Lin said. “We are working to validate our sensor against existing medical devices.”
While the device was primarily evaluated for its ability to monitor cardiovascular functions, researchers also demonstrated that the patch can be applied to the abdomen to monitor the diaphragm or to the extremities to monitor peripheral arteries. “The system has the potential to perform measurements at multiple points in the body, and we can easily adapt the probe design to fit various tissue monitoring requirements,” Xu said.
“With this type of device, we hope to blur the line between home care and hospital diagnosis,” Lin said. “We envision a future where diagnostics can be performed anytime, anywhere, thanks to wireless devices like these.”
This study was supported by a NIBIB grant (R01EB033464).
Study reference: Lin, M., Zhang, Z., Gao, X. et al. A fully integrated portable ultrasound system for monitoring deep tissues in moving subjects. Nat Biotechnology (2023). https://doi.org/10.1038/s41587-023-01800-0