Navigating the brain’s labyrinthine vasculature with standard surgical instruments can be incredibly challenging, even for the steadiest of hands. But with some robotic assistance, neurosurgeons could operate much more easily.
Researchers at Johns Hopkins University and the University of Maryland have laid the foundation for a soft robotic tool and control system that could give surgeons an unprecedented degree of maneuverability within the brain. A recent study published in the International Journal of Computer Assisted Radiology and Surgery demonstrates that the new system is both intuitive and very precise. Early results suggest that, with further development, the robot could one day speed up and improve the effectiveness of minimally invasive surgeries for life-threatening brain aneurysms and other serious conditions.
One of the common approaches to treating a brain aneurysm (a weakened blood vessel that swells and fills with blood) involves passing a plastic tube called a catheter through an artery, usually in the groin, with the goal of reaching and sealing the aneurysm without causing perforations along the way.
To address the twists and turns of the vasculature, doctors can bend the tips of the catheters in the desired direction before inserting them. Then, using their hands, they rotate the catheter as needed while pushing it into the aneurysm. But this approach has a major drawback.
“With regular catheters, you can’t bend the tip in a different direction as needed once inserted, which causes problems if an aneurysm is difficult to reach,” said study co-author Ryan Sochol, Ph.D., a professor of mechanical engineering at the University of Maryland. “This particular problem appears to be fairly consistent among neurosurgeons and others who perform endovascular interventions.”
After listening to neurosurgeons and studying surgical procedures, the authors of the new study concluded that a steerable robotic tool could greatly improve the process.
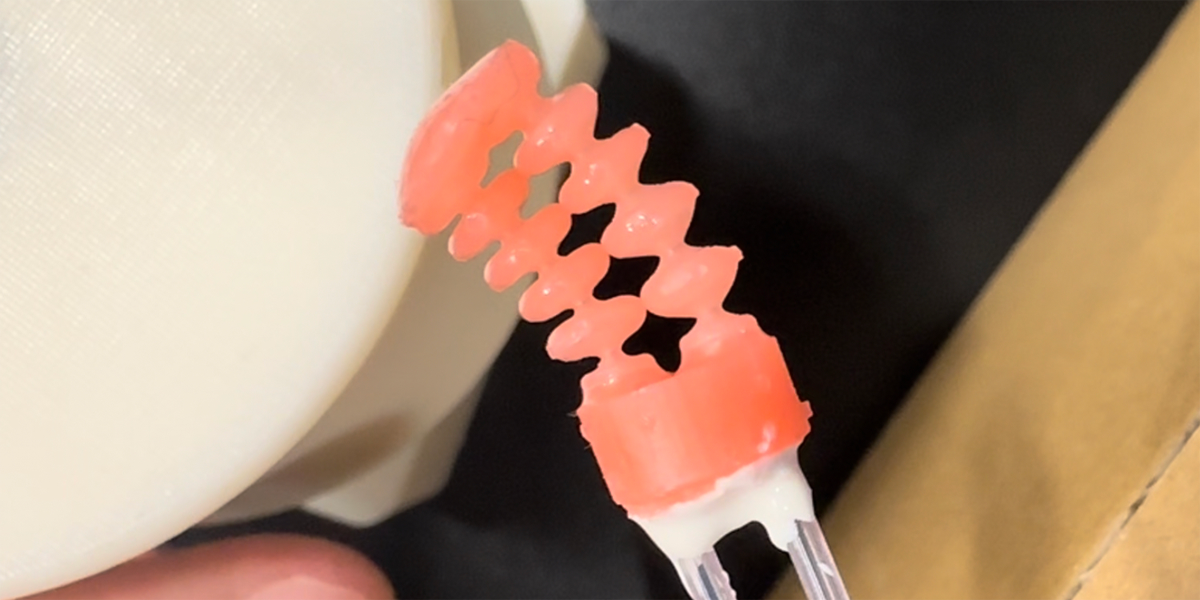
The researchers designed an air pressure (or pneumatic) operated catheter tip that they 3D printed using a soft, flexible resin. The design includes two hollow channels that run parallel along the tip and, if individually pressurized, cause the tip to deflect to the left or right.
While the tip of the catheter itself was inspired by existing designsThe authors sought to address a need that those previous robotic systems had not yet addressed: a control system that would fit well into today’s clinical workflow.
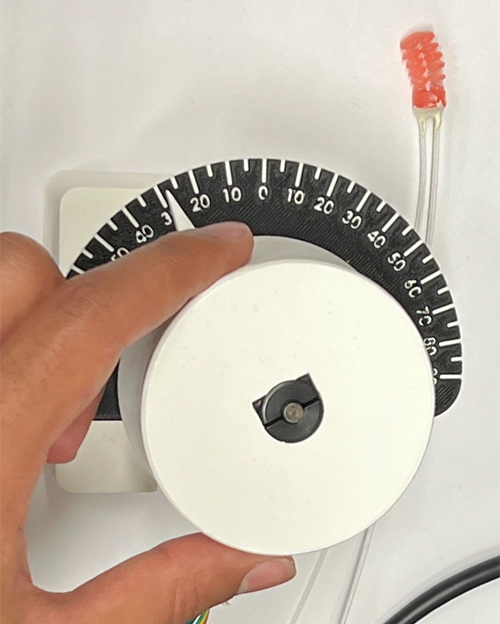
To provide clinicians with a similar but improved method, the team developed a manual dial that allows precise adjustments of the tip position, providing more control than rotating a pre-bent tip. Additionally, the dial offers haptic feedback that indicates when the tip is bent. With this system, researchers provide the ability to simultaneously move a catheter forward with one hand while adjusting the angle of the tip with the other.
To evaluate the device’s performance, the authors asked two users (one expert neurosurgeon and one with no prior surgical training) to adjust the position of the robotic tip to hit a series of five 2-millimeter-wide cylindrical targets spaced less than 2 millimeters apart.
Over 80 trials each, users guided the catheters into the barrels with one hand and operated the dial with the other, bending the tips even closer to each target.
The authors tracked how far the tips were from the goals and the time it took users to complete the tasks. The surgeon was clearly faster and more precise; However, after several tests, the rookie began to close the gap, almost matching his counterpart’s accuracy.
“Both users were able to use the robotic system for submillimeter precision control, which is smaller than the two millimeter diameter of cerebral vessels and aneurysm openings in the brain,” said senior author Axel Kreiger, Ph.D., a professor of mechanical engineering at Johns Hopkins University. “Overall, it was really nice to see that the results support the viability of the system.”
Now that the study gives them more momentum, the authors are eager to continue developing the robotic tool with plans to shrink it to a more clinically relevant size and test it against targets in more anatomically precise environments, Krieger explained.
In the future, the authors also aim to increase the functionality of their design by adding tips in series, which could allow the device to bend into more complicated shapes and navigate difficult vascular environments.
“The soft tip of the microcatheter is very innovative and could be key to the widespread use of robotics in endovascular surgery,” said Moria Bittmann, Ph.D., director of the NIBIB Robotics Program.
This research was funded by a grant from NIBIB (R01EB033354), the Maryland Robotics Center, and the Center for Engineering Concept Development at the University of Maryland.
This Science Highlight describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Noah Barnes et al. Towards a novel soft robotic system for minimally invasive interventions. International Journal of Computer Assisted Radiology and Surgery (2023). DOI: 10.1007/s11548-023-02997-w