For most of our tissues and cells, lack of oxygen or hypoxia is bad news. Cancer cells, on the other hand, can thrive in these hypoxic conditions, making tumors less susceptible to cancer treatments, including radiation. Now, new research may offer a way to break down cancer’s hypoxia-induced defenses.
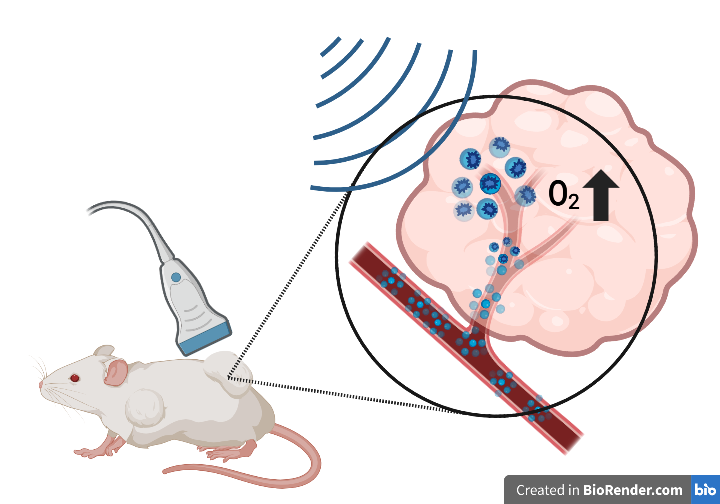
A team led by researchers at Thomas Jefferson University and Drexel University has devised a strategy that combines ultrasound with microbubbles to deliver oxygen and anti-cancer drugs to tumors. The results of a study published in the magazine Pharmacy indicate that the method, tested in mice, primed tumors to be more vulnerable to radiotherapy, resulting in slower tumor growth and longer survival. The study authors suggest that, with further development, their approach could be used to improve the effectiveness of radiotherapy in the clinic for a variety of cancers.
“At this time, there is very little we can do clinically to overcome hypoxia in radiation therapy, despite it being a well-known and documented limitation,” said study author John Eisenbrey, Ph.D., associate professor of radiology at Thomas Jefferson University. “The hope is that a more localized, more aggressive approach to hypoxia, like what we’ve done here, will overcome some of that.”
A long-standing staple of cancer treatment, radiation therapy, also called radiotherapy, is used to treat more than half of all cancer patients. With this method, doctors use high doses of radiation to kill cancer cells.
But many tumors are resistant to radiation therapy, and hypoxia is a major reason, Eisenbrey said.
“Every time I say we’re delivering oxygen to tumors, a lot of people say, ‘Well, that’s crazy. You’ll encourage them to grow,'” said study co-author Margaret Wheatley, Ph.D., a professor of biomedical engineering at Drexel University. But radiation therapy, which prevents cancer cells from replicating, requires an ample supply of nearby oxygen to be effective, he explained.
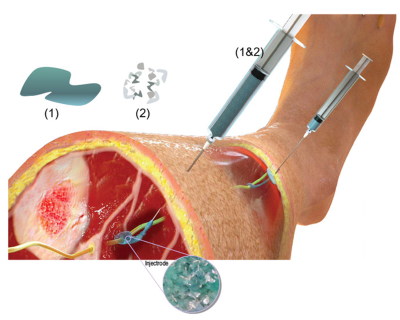
With the goal of overcoming resistance to radiation therapy, Wheatley, Eisenbrey and their colleagues designed a method that sensitizes tumors to radiation therapy using tiny, delicate bubbles (called microbubbles) that are about the size of red blood cells.
To increase oxygen levels in the tumors, they packed oxygen molecules into microbubbles. And to prevent cancer cells from consuming oxygen for their own benefit, they also added the drug lonidamine, which disrupts the metabolism of cancer cells.
After assembly, the microbubbles are injected and circulate throughout the body, releasing their payload only at the intended target, preserving healthy tissues. The trick to selective release is ultrasound. By specifically launching ultrasound waves at a tumor, researchers can cause the microbubbles that have traveled there to burst and release their contents.
In a previous studyThe researchers used the method to treat mice with tumors derived from breast cancer cells, with favorable results. They upped the ante on the new work and instead worked against tumors derived from head and neck cancer cells.
“They are noticeably more hypoxic than other solid tumors and also relatively resistant to radiation therapy,” Eisenbrey said.
The study authors injected mice with microbubbles containing oxygen and lonidamine, blasting them at the tumor site with ultrasound, while also administering a drug called metformin, known to slow cancer growth, orally. Other groups of mice were given less than the full treatment and did not receive one or many of the elements of the preradiotherapy strategy.
After exposing the animals to radiation, the researchers tracked the size of the tumors over the next three months.
All groups that received some degree of treatment experienced varying levels of slower tumor growth. Mice treated with fully loaded bubbles and metformin before radiation therapy lived longer and the growth of their tumors slowed dramatically. The authors suggest that the reason is that increased oxygen within the tumors made them more vulnerable to radiation treatment.
Gaining ground in head and neck cancer is a very encouraging result, even in mice, Eisenbrey said. However, the team intends to continue refining the method by optimizing radiation and drug doses for better results and streamlining microbubble manufacturing, ultimately bringing their solution closer to reality for cancer patients.
“The authors are using ultrasound and microbubbles in an innovative way, delivering oxygen and drugs to address a very serious clinical dilemma. They had some promising results, so I’m curious to see how this approach fares with further development,” said Randy King, Ph.D., director of the ultrasound program in the Division of Applied Science and Technology at the National Institute of Biomedical Imaging and Bioengineering (NIBIB).
This research was funded by a NIBIB grant (R01EB026881).
This Science Highlight describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Quezia Lacerda et al. Improved tumor control after radiosensitization with ultrasound-sensitive oxygen microbubbles and inhibitors of tumor mitochondrial respiration in a preclinical model of head and neck cancer. Pharmaceutical (2023). DOI: 10.3390/pharmacéutica15041302.