Each year, thousands of Americans, mostly over the age of 75, need their aortic valve replaced. Now, patient-specific 3D printed aorta models can aid in presurgical planning and improve outcomes of minimally invasive valve replacement.
The left ventricle of the heart has the important function of pushing fresh, oxygenated blood into the aorta, which then distributes it throughout the body. The aortic valve opens as blood passes through and then closes so blood cannot flow back toward the heart. Aortic stenosis is a condition in which the aortic valve narrows over time, causing the heart to work harder, a condition that can lead to heart failure.
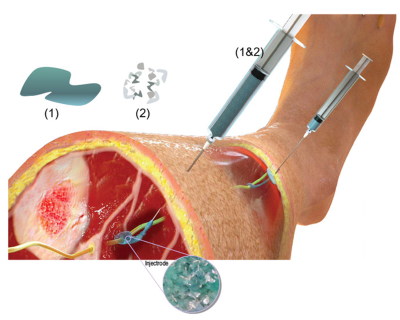
Transcatheter aortic valve replacement (TAVR) is a procedure in which an artificial heart valve is inserted with a catheter through the aorta and expanded (like opening an umbrella) to replace a defective aortic valve. TAVR is increasingly used because it is a minimally invasive procedure that is much safer than open heart surgery for the predominantly elderly patients who require the procedure. However, due to the irregularities of the diseased valve and the patient-specific contours of the aorta, a perfect leak-proof fit and optimal positioning of the new valve is not always guaranteed.
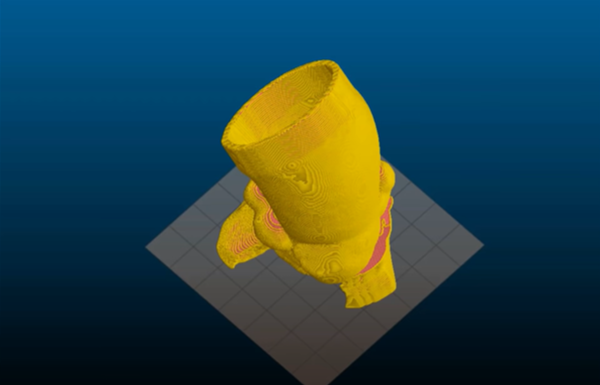
Now, NIBIB-funded engineers at the University of Minnesota, led by Michael McAlpine, who holds the Kuhrmeyer Family Chair in the Department of Mechanical Engineering at the University of Minnesota, have made significant progress toward improving TAVR by 3D printing an accurate model of a patient’s diseased valve and surrounding parts of the aorta. This physical model of the region, known as the aortic root, allows doctors to practice the procedure needed for each patient, allowing them to identify the correct size replacement valve and determine the exact location in the aorta that will provide the best fit and function.
“As the U.S. population ages, the number of people over age 75 requiring valve replacement through TAVR will continue to grow,” explained Michael Wolfson, NIBIB program director on bionic systems. “The ability to create patient-specific aortic root models is an important advance that could improve the success rate of this challenging procedure and significantly reduce the risks of postoperative complications.”
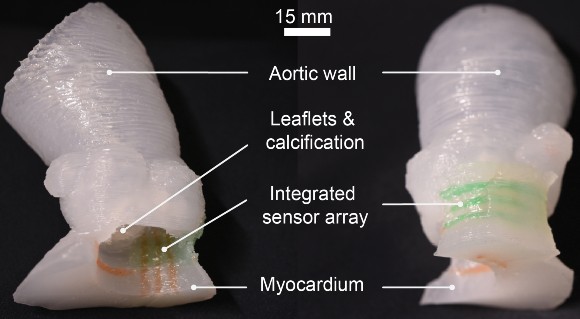
Although aortic root models have been used before for surgical planning, models created using the advanced 3D printing technique are much more realistic in texture and elasticity. Another unique aspect of these models is the incorporation of sensors in the wall of the aorta. The sensors provide feedback that allows doctors to prevent the replacement valve from applying excessive pressure to the conduction pathway that controls heart rhythm. Too much pressure can cause abnormal heart rhythms and the immediate need to implant a permanent pacemaker in the patient.
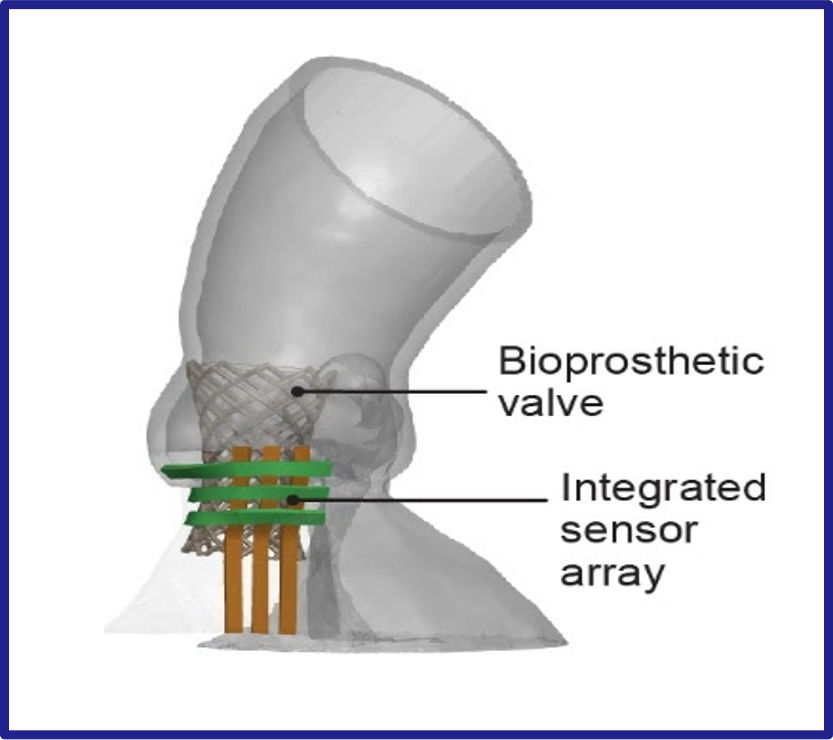
The engineering team uses CT scans of the patient’s heart to recreate the exact shape of the aortic root region. They are then 3D printed with specialized silicone-based inks that match the feel of real heart tissue. Soft electrical sensors that give pressure feedback are also 3D printed on the model and are made of a conductive hydrogel.
“This 3D printing process was designed to help doctors improve the outcomes of the TAVR procedure and can also help give patients a clearer understanding of their anatomy and how the procedure works,” McAlpine said. As engineers continue to improve 3D printing techniques and create even more realistic organ models, McAlpine imagines where such technologies could lead. “In the future, as our 3D printed models incorporate more aspects of organ function, we see the potential for the models themselves to one day be used as artificial replacement organs.”
The work was published in the journal Science Advances.1. Funding was provided through grants from the National Institute of Biomedical Imaging and Bioengineering (DP2EB020537), Medtronic plc, and the MnDRIVE program at the University of Minnesota.