Deep brain stimulation (the application of electricity to specific deep regions of the brain to modulate its function) has been used clinically for more than 25 years. This technique is used to monitor and treat neurological conditions, especially movement disorders, such as parkinson’s disease and epilepsy. However, many of these interfaces are highly invasive, as they require removing part of the skull to implant electrodes in the brain. Finding a way to monitor and stimulate the central nervous system in a less intrusive way has been a holy grail for those working in the field of neuromodulation.
Now, a collaborative team of NIH-funded researchers from Rice University and the University of Texas is developing a method to access and stimulate deep regions of the brain without drilling a hole in the skull. They designed a small pulse generator that can be implanted in the spine after a lumbar puncture. This pulse generator is connected to a stimulating catheter, which can be guided through the cerebrospinal fluid to the surface of the brain. Following preliminary experiments on human cadavers, the team successfully used the device to record and stimulate brain activity in sheep with the help of a wireless interface. His work was recently published in Nature Biomedical Engineering.
“Using our technique, we showed that it is possible to place an electrode in the brain using a relatively simple lumbar puncture, avoiding the need for a craniotomy,” said study author Jacob Robinson, Ph.D., professor of electrical and computer engineering at Rice University. “By reducing the invasiveness of deep brain stimulation, we hope our research will help reduce the barriers to this technology and one day provide improved therapies for patients with neurological disorders.”
Deep brain stimulation devices typically consist of two main components: an electrode, which is in direct contact with the brain, and an implantable pulse generator, which controls the electricity delivered to specific regions of the brain. Traditional pulse generators for deep brain stimulation are implanted under the skin near the collarbone and require a battery; Electrodes are usually inserted through holes in the skull to reach the necessary brain regions.
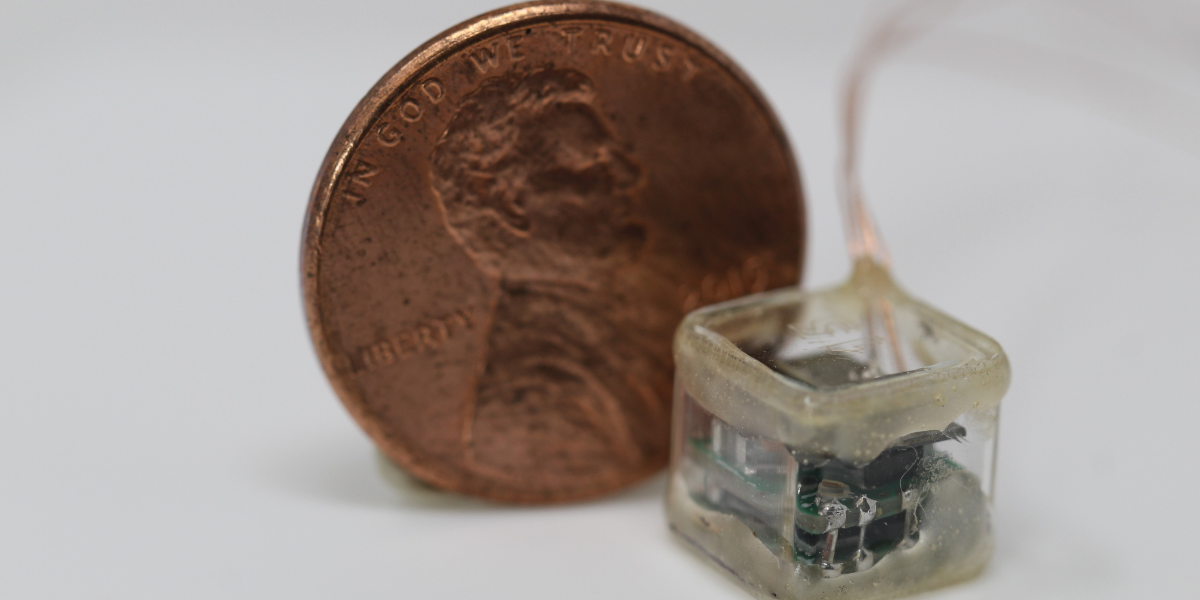
The proof-of-concept neuromodulation device described in this research contains the same basic components, but they have been optimized to reduce the invasiveness of traditional deep brain stimulation interfaces. The implantable pulse generator has been miniaturized, measuring approximately 1 cm in each dimension and does not require a battery; Instead, the device works with magnetoelectric films, which can be activated by an external magnetic field. And rather than drilling into the skull to place an electrode, researchers have developed a method to slide a stimulation catheter through the endocisternal space, or the tubing that carries cerebrospinal fluid throughout the central nervous system. This technique allows the team to place electrodes in the brain using a minimally invasive approach, which could potentially improve the safety and recovery time of deep brain implantation. Both the pulse generator and the electrode could enter the body through a small incision in the lumbar spine, in the lower back.
“The brain has several ventricles, or fluid-filled cavities, that lie deep in the brain, and these ventricles connect to other regions of the brain and spinal cord through a series of tubes,” explained study author Peter Kan, MD, a neurosurgeon at the University of Texas Medical Branch. “With the help of X-ray imaging, we can use these fluid-filled tubes to carefully direct the electrode up the spine and into specific deep regions of the brain, all without having to open the skull.”
The researchers first evaluated their method on human cadavers and found that they could insert the stimulation catheter into the spine and successfully guide the electrode to specific regions deep in the brain. Next, the researchers wanted to evaluate how well their device could stimulate deep regions of the brain in a live animal. To do this, they turned to a common model used in research on the human spine: the sheep.
After implanting the pulse generator in the lower spine and guiding the electrode into the sheep brain, the researchers used an external magnet to wirelessly activate the neural interface. As expected, the researchers were able to stimulate the motor cortex, as evidenced by muscle contractions in the animals’ hind legs. Furthermore, the researchers showed that they could stimulate deep regions of the brain and subsequently detect the corresponding activation of the central nervous system through evoked potentials (or electrical signals) measured in the spinal cord.
“We also showed that we can place two electrodes, one in the animal’s brain and the other in the spinal cord, and activate them simultaneously,” Robinson explained. “Multisite access allows for coordinated activation of multiple regions of the central nervous system, which is an important technique in neuromodulation therapies.”
The researchers evaluated the long-term viability of the device in two of the 12 sheep. After 30 days, they found that the implant was still able to effectively stimulate the central nervous system. What’s more, the animals did not present any neurological deficit.
“This device, although still in an early phase of development, has the potential to bring neuromodulation implants to more patients, making deep brain stimulation devices as common as cardiac pacemakers,” said Moria Bittmann, Ph.D., program director in NIBIB’s Science and Technology Discovery Division. “Future work will ensure the technology is safe before it is evaluated in humans.”
This study was supported by a NIBIB grant (U18EB029353).
This prominent scientist describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Chen, JC, Dhuliyawalla, A., García, R. et al. Endocisternal interfaces for minimally invasive neuronal stimulation and recording from the brain and spinal cord. Nat. Biomedical. ing (2024). https://doi.org/10.1038/s41551-024-01281-9