Obtaining a biopsy is often an important first step in diagnosing and treating cancer. But brain tumors present unique challenges: To perform a biopsy, a neurosurgeon will likely need to drill a hole in the skull, and removing brain tissue can cause complications, such as bleeding, swelling of the brain, or infection. Promising methods for diagnosing brain tumors non-invasively have remained elusive…until now.
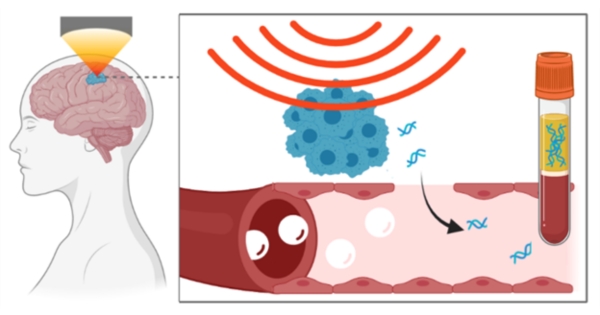
A collaborative team of NIH-funded researchers is developing a way to obtain DNA shed from brain tumors using focused ultrasound. His first study in humansreported in the Nature diary npj Precision Oncologycould be an important step towards improving the way brain tumors are diagnosed.
“Focused ultrasound is conventionally used as a therapeutic technique, in which high-intensity ultrasound waves are directed to a single focal point to destroy problematic tissue,” explained Randy King, Ph.D., program director of NIBIB’s Division of Applied Science and Technology. “The method described here turns that paradigm on its head, leveraging focused ultrasound not for treatment, but for a diagnostic purpose.”
Sonobiopsy: focused ultrasound joins liquid biopsy
Traditional biopsy approaches involve cutting into the body to remove a sample of suspicious or cancerous tissue, which is then analyzed to direct treatment approaches. However, tumors can release fragments of their DNA into the bloodstream, which can also be collected and analyzed. This approach, known as liquid biopsyIt is used clinically for some types of cancer and has several advantages, such as the ability to sample tumor DNA non-invasively many times.
However, it is very difficult to capture DNA shed from tumors in the brain. The brain is surrounded by a protective vascular network known as the blood-brain barrier, which prevents the passage of certain substances. This barrier works in both directions: Potentially harmful molecules cannot enter easily, and materials in the brain cannot easily leave either.
Enter sonobiopsy. This technique uses focused ultrasound to mechanically disrupt the blood-brain barrier, allowing small molecules (such as tumor DNA) to pass through. Once in the bloodstream, tumor DNA can be collected through a simple blood draw and analyzed to gather information about a patient’s cancer.
“The concept of using focused ultrasound to temporarily open the blood-brain barrier is not new; in fact, it has been in development for more than two decades,” explained study co-senior author Hong Chen, Ph.D., an associate professor at Washington University in St. Louis. “But these efforts have largely focused on opening the blood-brain barrier to allow drugs to enter the bloodstream. in the brain to treat brain diseases. Our team is trying to get molecules. outside the brain, specifically the DNA released from brain tumors.”
The opening of the blood-brain barrier by focused ultrasound depends on the presence of microbubbles. These microbubbles are FDA-approved contrast agents that are traditionally used to enhance ultrasound imaging techniques. They can circulate through blood vessels throughout the body, including those around the brain. When microbubbles are exposed to acoustic pressure, such as focused ultrasound waves, they expand and contract. Subsequently, the repeated expansion and contraction of the microbubbles pushes and pulls on the vessel walls. This mechanical force puts pressure on the blood-brain barrier, improving the permeability of blood vessels and ultimately allowing small molecules to enter or leave the brain.
Evaluation of sonobiopsy in a first clinical trial in humans
In this study, the researchers introduced a compact focused ultrasound device that can be seamlessly integrated into existing clinical workflow. Your first human being clinical trialLed by study co-senior author Eric Leuthardt, MD, Shi Hui Huang Professor of Neurosurgery at the University of Washington School of Medicine, evaluated the sonobiopsy device in five patients with high-grade gliomas, an aggressive type of tumor that develops in the brain. Each of these patients was scheduled to undergo brain surgery to remove their tumors. Immediately before surgery, the researchers performed a sonobiopsy by directing focused ultrasound waves directly at the brain tumor. Blood samples were collected before and after the procedure, and patients then had their tumors removed. Both blood samples and the removed tumor tissue were analyzed after surgery.
Using tumor tissue removed from the brain, the researchers were able to identify tumor-specific DNA sequences for each patient. They used this information to determine whether the DNA found in the bloodstream after the sonobiopsy procedure originated from the tumor in the patient’s brain. Their analyzes revealed that sonobiopsy significantly improved the detection of tumor-specific DNA in the bloodstream in three of the five patients. In particular, in one patient, the amount of tumor DNA detected in the bloodstream almost doubled.
“We are still in the development stage of this technology, and our trial was designed to use tumor tissue removed from the brain as a reference point to determine whether DNA found in the bloodstream was shed from the tumor after the sonobiopsy procedure,” Leuthardt explained. “After fully validating our method, the ultimate goal is to use sonobiopsy to non-invasively analyze lesions in the brain to understand their molecular and genetic makeup to guide treatment decisions.”
Although sonobiopsy did not increase tumor-specific DNA in the bloodstream among the five patients, Chen said this finding was expected. “Because this is the first human trial, the ultrasound parameters we used were probably not optimal,” he said. “We erred on the side of caution to ensure that the ultrasound parameters were as safe as possible for our patients. Given this approach, the fact that the procedure resulted in an increase in circulating tumor DNA in more than half of our patients was very encouraging.”
In terms of safety, the researchers did not observe any detectable tissue damage on the surface of the brain after the sonobiopsy procedure, and microscopic analysis of the removed tumor tissue did not reveal any apparent lesions in the regions exposed to focused ultrasound.
“In addition to demonstrating the feasibility of our approach, this prospective first-in-human trial suggests that sonobiopsy has the potential to transform the precision diagnosis of brain tumors and other neurological disorders,” Chen said. “While our early data are promising, further studies with larger samples are needed to confirm these initial findings and establish the clinical utility of sonobiopsy.”
Study reference: Yuan, Jinyun et al. “First-in-human prospective trial of sonobiopsy in patients with high-grade glioma using neuronavigation-guided focused ultrasound.” NPJ Precision Oncology vol. 7.1 92. September 16, 2023, doi:10.1038/s41698-023-00448-y
This study was supported by grants from NIBIB (R01EB027223 and R01EB030102), the National Cancer Institute (NCI; R01CA276174), the National Institute of Mental Health (NIMH; R01MH116981 and UG3MH126861), and the National Institute of Neurological Disorders and Stroke (NINDS; R01NS128461).