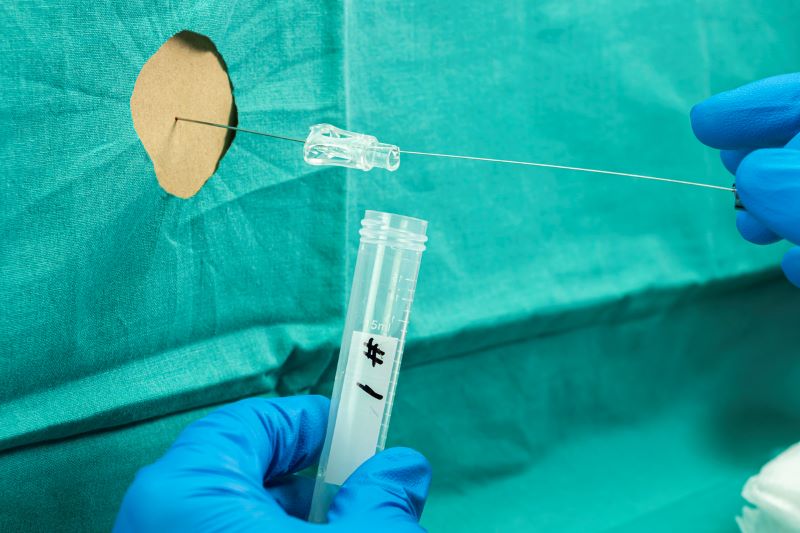
A lumbar puncture, also known as a lumbar puncture, is a common clinical procedure that uses a hollow needle to penetrate the spinal canal and access the cerebrospinal fluid that surrounds the brain and spinal cord. This procedure is used to diagnose serious nervous system conditions such as meningitis or encephalitis or to inject anesthetic medications or chemotherapy.
Doctors often refer to lumbar punctures as “blind bedside procedures” because they have to use their hands to feel the space between two lumbar bones and then try to insert the needle in the right place. Finding the gap can be particularly difficult in overweight or elderly people.
“In some patients undergoing a lumbar puncture, the bone points used to guide the needle are not easily felt, and in the elderly, there is spinal degeneration, which makes this procedure challenging,” explained Abhay Moghekar, MBBS, associate professor of neurology and director of the Brain Fluid Center at Johns Hopkins Hospital.
“Multiple futile attempts can be painful for the patient and lead to a high probability of blood contamination of the cerebrospinal fluid, which could affect the interpretation of various diagnostic tests for life-threatening diagnoses such as meningitis, encephalitis or subarachnoid hemorrhage,” he said.
Moghekar and a team of researchers from Johns Hopkins University and Clear Guide Medical, Inc., a company specializing in imaging devices, developed a new ultrasound navigation system that could provide accurate, real-time and intuitive planning and guidance of needle insertion for lumbar puncture procedures. The results of your preclinical study were published in IEEE Transactions on Medical Robotics and Bionics.
The needle navigation system integrates three components that would allow the doctor to insert the needle more accurately: a cellphone-sized ultrasound imaging scanner that could be attached to a patient’s skin along the lower spine, imaging algorithms that estimate bone surfaces, and augmented reality where a digital screen to guide needle insertion is overlaid on the patient’s view of the spine.
“This portable ultrasound navigation system has several advantages over other imaging navigation methods. A preoperative CT scan would not be necessary, and doctors could use both hands to control the needle when using the navigation system. They currently use one hand to hold and guide the imaging probe and the other to insert the needle,” said Peter Kazanzides, Ph.D., research professor of computer science. at Johns Hopkins University and corresponding co-author of the paper.
NIBIB funds small business research and development
The collaborative study was funded by the NIBIB Small Business Innovation Research (SBIR) program, a federal initiative that supports research with high potential for technology commercialization.
“This funding helped us explore research ideas that we normally wouldn’t be able to pursue unless we saw immediate commercial benefits,” said co-author Purnima Rajan, Ph.D., principal investigator on the SBIR-funded project and senior research engineer at Clear Guide Medical, Inc.
The SBIR program reflects NIBIB’s mission by supporting innovative technologies through various stages of research and commercial development. The program is divided into multiple phases, with the first phase focusing on the feasibility of the project.
The current study is based on previous research funded by a Phase 1 grant from SBIR showing that the system’s ultrasound scanner significantly improved visibility of the lumbar space.
Evaluation of augmented reality navigation system
In the current study, the researchers first evaluated the overall accuracy of the navigation system by comparing two forms of augmented reality (a tablet with camera-based tracking or a head-mounted display similar to immersive glasses, worn by the doctor, with optical tracking).
Both types of augmented reality precisely guided the placement of the needle to its target. The overall needle navigation accuracy was 2.83 mm for the tablet method and 2.76 mm for the head-mounted display method. The results were within the 4 mm benchmark used in spine surgery for precise needle placement.
The researchers then conducted a preliminary user study to compare the two augmented reality navigation systems and obtain feedback. A total of 16 users completed eight series of lumbar puncture procedures using a realistic anatomical model (phantom) of the spine.
Users were successful 89% of the time when first inserting the needle into the lumbar phantoms. Users were able to reach the targets with an average of 1.14 and 1.12 needle insertion attempts using the head-mounted display and tablet navigation systems, respectively. In the present study, a successful puncture insertion was defined when the tip of the needle reached the target location, in this case, a rubber tube embedded in the canal of the phantom vertebrae.
In comparison, other patient studies have shown that the traditional palpation method for needle insertion may require multiple needle insertion attempts. a study demonstrated that while the first needle insertion was successful in 71% of patients, almost 30% of patients required multiple insertion attempts or insertion failed.
Additionally, users preferred the ease of the Clear Guide Medical tablet-based navigation system to the head-mounted display.
A limitation of the preliminary study was that most users were not familiar with using ultrasound imaging or augmented reality applications and only one physician was included. However, the researchers plan to test the system with doctors in the next phase.
Looking to the future
“Our team at Hopkins is very excited about the direction we are taking toward portable ultrasound devices. Our device can capture the complex shape of lumbar bones without the shadows often seen in typical ultrasound scanners and has the flexibility to adapt to movement,” said Emad Boctor, Ph.D., co-corresponding author of the paper and research associate professor at the Computational Sensing and Robotics Laboratory at Johns Hopkins University.
Rajan added that since the study was completed, researchers have replaced their method of tracking needles using QR and other codes with artificial intelligence, which will eventually make them easier for doctors to use.
Boctor, who is also co-founder of Clear Guide Medical Inc., said the next step is for the team to apply for the NIBIB SBIR Phase 2 grant to develop the product for commercialization. That phase will focus on clinical evaluation and acceptance.
“Given the promising results of the Phase 1 study, we look forward to taking the next step in the development of the portable ultrasound navigation system. The advances made in navigation accuracy could ultimately benefit patients needing lumbar puncture procedures,” said Randy King, Ph.D., program director in NIBIB’s Division of Applied Science and Technology.
This study was supported in part by a grant from NIBIB (R43EB031731) and the National Science Foundation.
This Science Highlight describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Jiang B, et al. Portable mechatronic ultrasound integrated AR navigation system for lumbar puncture guidance. IEEE Transactions on Medical Robotics and Bionics. (2023). DOI: 10.1109/TMRB.2023.3319963.