Heart disease is the leading cause of death worldwide. In the US it is estimated that someone dies every 34 seconds of cardiovascular diseases. Diagnosing heart disease remains challenging as most methods only provide a snapshot of heart function, which may not be representative of overall heart health. Improvements in diagnostic technologies could help detect heart disease at earlier stages, potentially preventing numerous deaths.
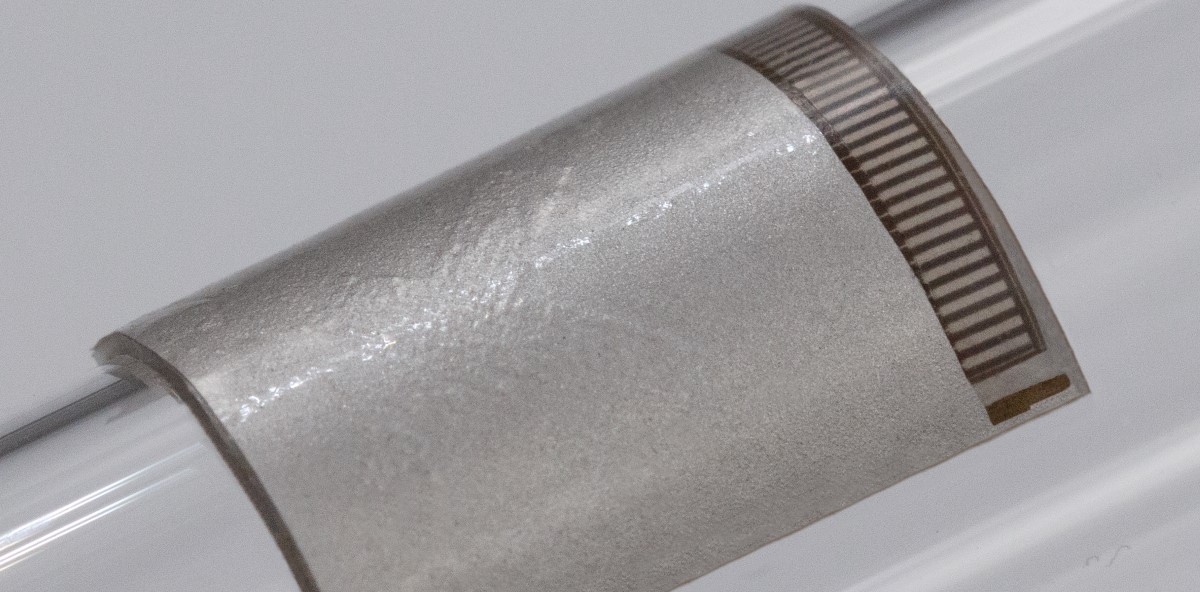
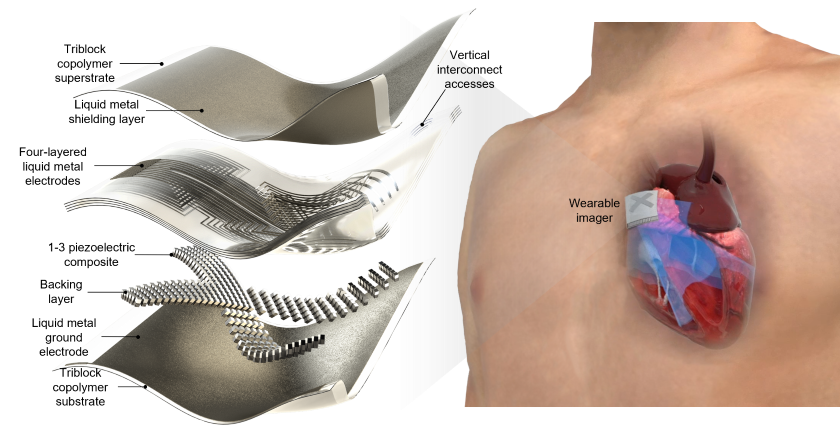
After years of research, an NIH-funded team has developed a portable cardiac ultrasound imager that can non-invasively capture real-time images of the human heart over an extended period. The patch, which is about the size of a postage stamp, has comparable performance to a commercial ultrasound device. What’s more, the imager can be used during exercise, providing valuable cardiac information when the heart is under stress. The prototype of the ultrasound patch was reported today in Nature.
“While existing wearable patches in development can capture things like heart rate and blood pressure, they are not designed to provide detailed information about cardiac function,” said Randy King, Ph.D., program director of NIBIB’s Division of Applied Science and Technology. “This innovative ultrasound device delivers critical information about the heart in real time, providing clinicians with detailed, actionable cardiac information. Combined with its slim design and stretchable properties, this patch could pave the way for continuous, non-invasive cardiac monitoring.”
Traditional cardiac ultrasound imaging requires physical rotation of the transducer so that a doctor can view and evaluate specific cross sections of the heart. This prototype patch, however, has two perpendicular piezoelectric assemblies that can be controlled independently. This allows the doctor to image multiple standard views of the heart without any intervention or repositioning of the patch. Liquid metal electrodes connect the small arrays so each element can be manipulated individually, and a type of silicone fills the inside of the device, making the entire patch highly stretchy and mitigating the need for an ultrasound gel. Together, these design elements allow the patch to maintain close contact with the skin at all times, overcoming the limitations of rigid ultrasound devices.
The researchers first needed to evaluate how their wearable patch compared to a traditional ultrasound device. Using a human tissue phantom model, they characterized the properties of their patch, such as its spatial resolution and signal-to-noise ratio, and found that these characteristics were similar to those of a commercial ultrasound device. They then used their patch to visualize the heart of a human subject. By looking at four standard views of cardiac anatomy, they found that the images generated by their patch were similar to those generated by the commercial ultrasound device.
After characterizing the performance of their patch, the researchers evaluated its usefulness during exercise, specifically, its performance during a stress test. Traditional stress echocardiography evaluates images of the heart before and after intensive exercise (since holding an ultrasound probe on the chest by hand and maintaining a stable position is impossible during exercise). The patch was used to monitor the cardiac performance of a healthy participant during a rigorous exercise session. The researchers found that the patch was able to capture the activities of the left ventricle (the chamber of the heart that pumps oxygenated blood throughout the body) without any interruption.
“Our patch allows us to evaluate the heart’s performance during exercise, providing valuable information about the heart when it is under a lot of stress,” explained the study’s senior author, Sheng Xu, Ph.D., an associate professor at the University of California, San Diego (UCSD). “This could allow real-time visualization of cardiac abnormalities as they manifest, which might go undetected under normal stress testing conditions,” he added. Additionally, the participant wore the patch for 24 hours without any allergies or skin irritation, illustrating its usefulness for all-day wear.
Finally, the researchers wanted to determine if their patch could be used to calculate key cardiac functions, such as stroke volume, cardiac output, and ejection fraction (all related to how much blood is pumped out of the heart and how efficiently it works). Using deep learning, they extracted specific features from ultrasound images taken with their patch and trained a model to reliably extrapolate these cardiac metrics. “The ability to non-invasively and continuously monitor such cardiac functions over a 24-hour period could revolutionize the field,” said Ray Wu, a graduate student in Xu’s lab and a co-author of this study.
An important next step in the development of this patch is to make it completely wireless. “As of now, our patch requires cables to supply it with power, control the piezoelectric transducers, and transmit the ultrasound data to a back-end system,” explained the study’s first author, Hongjie Hu, Ph.D., a postdoctoral researcher at UCSD. “Our immediate goals are to build an integrated power source for our patch and develop a wireless communication system between the patch and a remote device, such as a central workstation,” he said.
“While this wearable ultrasound patch may be in the early stages, its potential to non-invasively provide comprehensive, real-time cardiac information could transform healthcare in the future,” Xu said.
This study was funded by grants from NIBIB (R21EB025521, R21EB027303 and R01EB033464).
Study reference: Hu, H., Huang, H., Li, M. et al. A portable cardiac ultrasound imager. Nature 613667–675 (2023). https://doi.org/10.1038/s41586-022-05498-z