Artificially causing (or inducing) labor is becoming increasingly increasingly commonHowever, this practice comes with risks and its level of success is difficult to predict. But now, new research may offer a way to help predict outcomes and improve the process.
Researchers at the University of Arkansas for Medical Sciences (UAMS) have devised a non-invasive method to accurately measure the electrical activity of the uterine muscles. The results of a recent clinical study, published in the journal Current research in physiologyshow that the signals measured in pregnant patients before induction are strongly linked to whether their labor lasted less or more than 24 hours. The authors indicate that doctors could use the method to learn how patients might respond to induction and use the information to develop more effective strategies for labor and delivery.
If the health of a pregnant person or her baby would benefit from starting labor earlier, health care providers may recommend inducing the process. through medication or other means. Without reliable monitoring tools, physicians rely heavily on physical examinations and their experience to inform their induction strategies.
With this approach, the time spent in labor varies greatly from patient to patient and there is also a risk that excessive doses of induction medication will cause harm.
“Sometimes women sit there for 36 hours after being induced and nothing happens,” said Hari Eswaran, Ph.D., professor of obstetrics and gynecology at UAMS. “We wanted to know when the uterus is ready for delivery. If we capture beforehand a physiological signature that indicates the chances of a successful induction, that information can be used to personalize the approach.”
In search of revealing clues, Eswaran and his co-authors previously developed the Superconducting Quantum Interference Device (SQUID) Array for Reproductive Assessment, or SARA for short.
Measuring the electrical activity of various parts of the body using techniques such as electromyography or EMG is routine in the clinic. However, electrical signals from the uterus weaken when they reach the surface of the skin, making them particularly difficult to detect.
Instead of directly measuring electrical activity, SARA takes a backdoor.
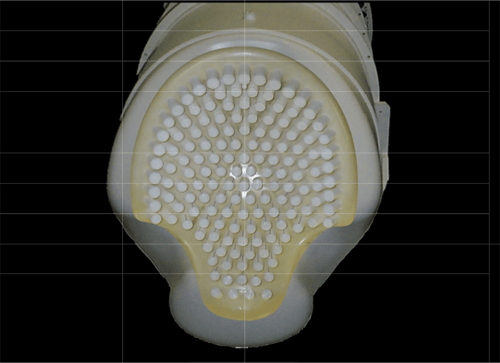
Electric current, whether it passes through electrical wires or the muscles of the human body, always generates a magnetic field around it. And if you can detect the field, then you can work backwards to calculate the electric current that produced it, Eswaran explained. This is the approach researchers are taking with SARA’s array of 151 biomagnetic sensors.
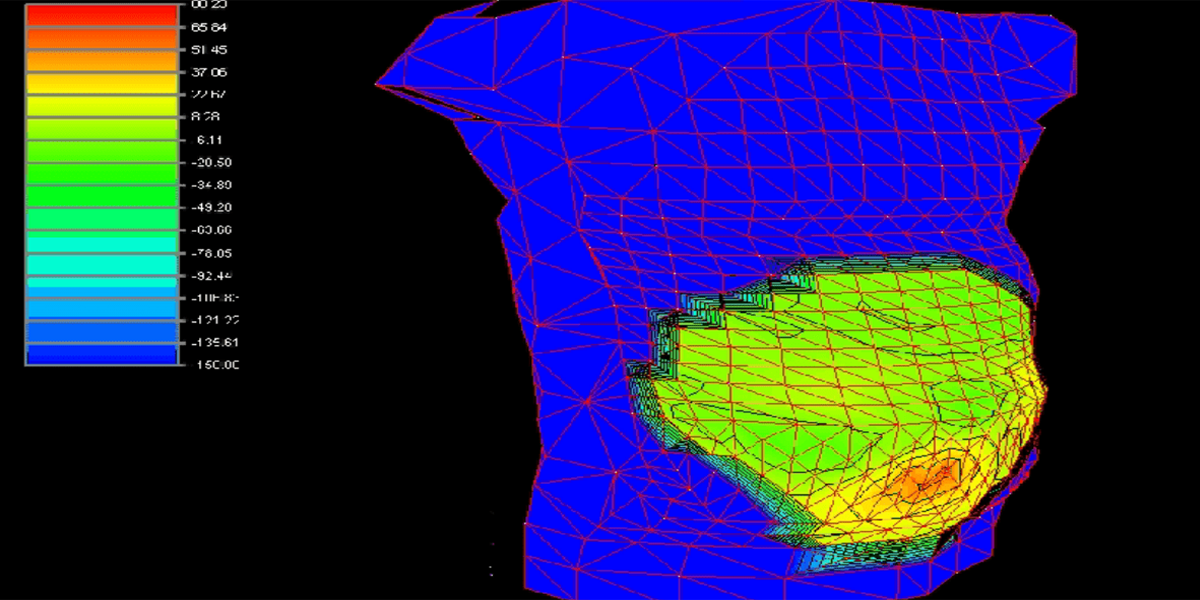
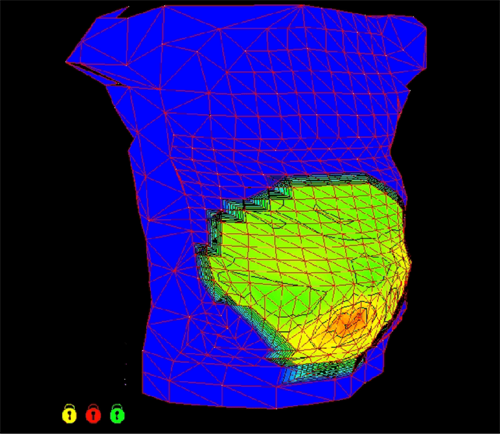
In the new study, the authors analyzed measurements taken from 27 patients who were between 37 and 42 weeks pregnant. Each person rested their abdomen on the SARA sensors, which recorded the magnetic activity produced by the uterus before induction. The authors converted the magnetic signals into metrics related to electrical activity, such as power. After looking at how long each patient took to give birth, the authors examined their data and detected a significant pattern.
Patients who delivered their babies within 24 hours of induction exhibited four times more uterine electrical energy across all recordings than those who were in labor longer.
While none of the patients experienced contractions while SARA recorded the signals, the results suggest that those with higher uterine electrical power were more prepared for delivery, Eswaran explained.
Equipped with a tool that could help predict induction responsiveness, physicians would be better informed when designing strategies tailored to each patient. With further research, SARA could become such a tool, potentially providing guidance on when to give induction medications and at what doses, leading to safer and more efficient labor and delivery.
“NIBIB awarded grants more than 15 years ago to support the development of new computational methods used in this clinical trial to predict labor contractions with SARA,” said Grace CY Peng, Ph.D., director of the NIBIB program in Mathematical Modeling, Simulation and Analysis. “It is very gratifying to see how this project demonstrates the translational potential of computational models to improve the quality of care in women’s health.”
This research was supported in part by a NIBIB grant (R01EB007264).
This Science Highlight describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Sarah Mehl et al. Evaluation of uterine electrophysiology before elective induction of labor. Current research in physiology (2023). DOI: 10.1016/j.crphys.2023.100103