What if bacteria, which love to grow deep in tumors, could guide cancer therapies directly to their target?
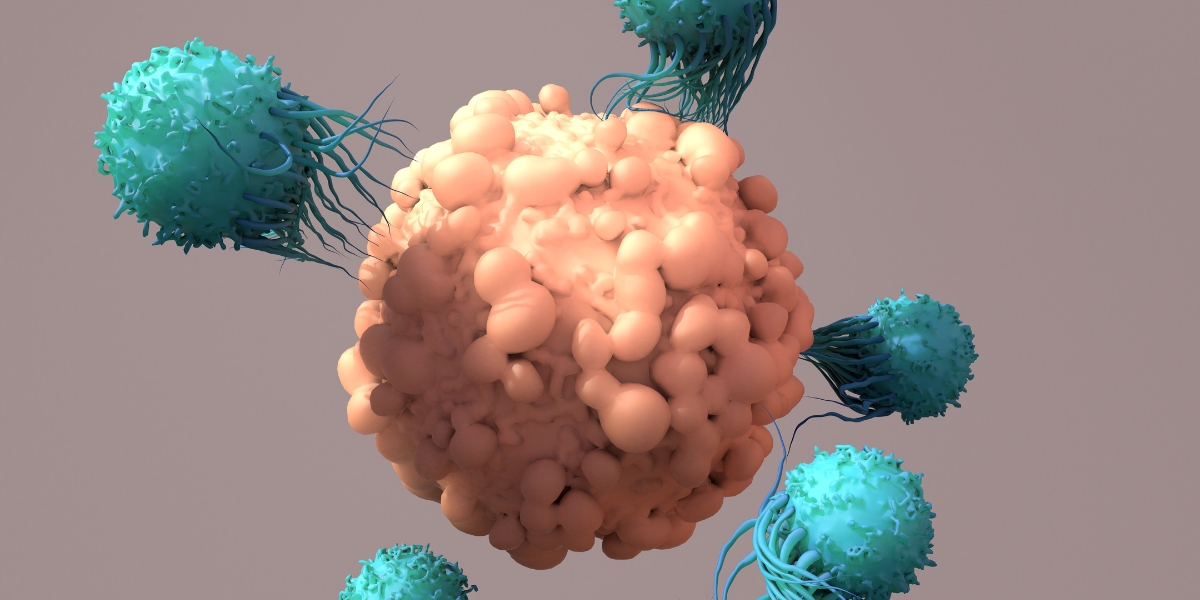
A team of researchers at Columbia University has engineered a bacterial strain to “light up” tumors and reprogram them. T cellsdrawn like a moth to the flame, it can find and destroy them. Its preclinical treatment, reported in Sciencecould potentially be effective against any type of solid tumor.
“While immunotherapy “The treatment described here takes advantage of the tumor-seeking behavior of bacteria to selectively mark cancer cells, allowing engineered T cells to effectively target a variety of solid tumors in mouse models. “This tumor-independent approach could potentially overcome a major limitation of current CAR T-cell therapies.”
CAR T cell treatment is a type of immunotherapy that modifies a patient’s own immune cells to better identify and attack cancer cells within their body. Here’s how it works: T cells, taken from a patient, are engineered to express an artificial protein called chimeric antigen receptoror CAR. These artificial receptors are designed to recognize a specific antigen It is found on the surface of a tumor cell. Once infused back into the patient, the CAR T cells can find the tumor by binding to these antigens, ultimately leading to the death of the cancer cells.
While CAR T cell therapy is currently used to treat several different types of blood cancers, it has not been approved to treat solid tumors. This is because a suitable solid tumor antigen for recognition by CAR T cells has not yet been identified. Tumors are heterogeneous, meaning that the expression of different genes (including antigens) is not the same among all tumor cells. This may limit the effectiveness of CAR T cell therapy or lead to cancer relapse.
Instead of relying on an antigen that may or may not be expressed on the surface of a tumor cell, research in Danino’s lab is taking a different approach. They are using an engineered bacterial strain, which selectively colonizes within the tumor core, to mark cancer cells with a synthetic antigen. These synthetic antigens act as a beacon, attracting CAR T cells that have been engineered to recognize them toward the tumor to effectively attack and destroy it.
“Tumor nuclei are especially susceptible to bacterial growth; things like low oxygen, low pH, necrotic tissue, and lack of immune cells constitute ideal conditions for bacterial colonization,” explained the study’s first author, Rosa Vincent, Ph.D. Taking advantage of these features, the study authors engineered a non-pathogenic bacterial strain to release a fluorescent tag that its CAR T cells could recognize. “After the bacteria grow to a critical population density, they all open simultaneously and release their payload, which marks the tumor tissue and directs the CAR T cells to them,” Vincent explained.
The researchers administered their engineered bacteria intratumorally (by directly injecting the bacteria into tumors) or systemically (administering the bacteria into the bloodstream) in several different mouse models. Both methods led to efficient tumor colonization and, more importantly, neither method led to bacterial growth in healthy organs. “During the course of our study, we did not see bacteria growing outside of tumors, even in mice with severely compromised immune systems,” Vincent said.
After the bacteria released their fluorescent antigen (approximately 48 to 72 hours postpartum), the researchers administered their engineered CAR T cells either intratumorally or systemically. After two rounds of CAR T cell administration, they found that their combinatorial treatment significantly reduced tumor growth in multiple mouse models, including breast and colorectal cancer models.
“In addition to their ability to selectively attack tumors, the bacteria are immunogenic and can initiate a robust immune response, which likely improves the efficacy of our treatment,” Vincent explained. Another benefit of using bacteria is their inability to easily grow outside the tumor, he added.
“Identifying selectable tumor-specific antigens has been a major hurdle in CAR T cell research, so our team decided to design a synthetic antigen and program a CAR that could recognize it,” explained the study’s senior author, Tal Danino, Ph.D., associate professor of biomedical engineering at Columbia University. “This bioengineering approach allowed us to circumvent a major bottleneck in the field.”
As this study was conducted in mice, the study authors point out that this experimental treatment is far from being evaluated in clinical trials. Additionally, because humans are much more sensitive to bacteria than mice, this combinatorial treatment will need to undergo rigorous safety studies before being tested in human patients.
This study was supported by a grant from NIBIB (R01EB030352) along with a grant from the National Center for Advancing Translational Sciences (NCATS; UL1TR001873).
This prominent scientist describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is critical to promoting new and better ways to prevent, diagnose, and treat diseases. Science is an unpredictable and incremental process: each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without knowledge of fundamental basic research.
Study reference: Rosa L. Vincent et al. CAR-T cells guided by probiotics to attack solid tumors. Science 382211-218 (2023). DOI:10.1126/science.add7034