NIBIB-funded engineers at UC San Diego have developed a flexible all-in-one epidermal patch that can simultaneously and continuously monitor cardiac output and metabolic levels of glucose, lactate, caffeine or alcohol. The patch is an important step toward continuous, non-invasive health monitoring of chronic diseases as well as early signs of disease development.
Devices capable of non-invasively detecting health status offer significant improvements in the treatment of chronic diseases such as diabetes and hypertension. A more ambitious goal is to detect indicators of disease onset, which will allow for early intervention that can prevent the development of a condition.
Now, a flexible skin patch sensor developed by engineers at the University of California, San Diego (UCSD) is the most sophisticated of this type of technology to date.
“The UCSD team has figured out how to put ultrasound sensors (which monitor heart rate and blood pressure) and chemical sensors (which detect glucose metabolites and other substances in body fluids) on the same small patch,” explained Randy King, Ph.D., director of the NIBIB program in Diagnostic and Interventional Ultrasound. “This is a great example of the type of innovative engineering that NIBIB supports and which has the real potential to have a huge impact on healthcare in the US and around the world.”
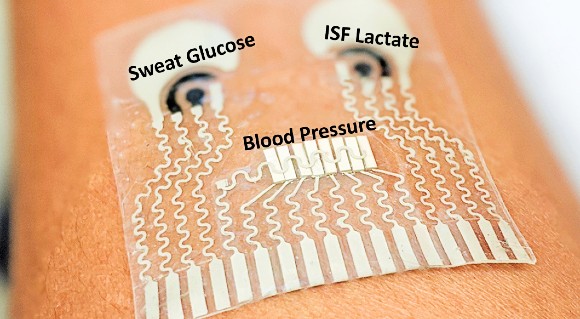
The two-by-two-inch elastic patch (and the electronic circuits printed on it) looks a bit like a cartoon character’s face with two big eyes and a mustache. The “left eye” is a chemical sensor that detects substances in sweat: lactate, which increases during exercise, as well as caffeine and alcohol. The “right eye” detects substances in the interstitial fluid (fluid in the space between the body’s cells), in this case, blood glucose levels. The “moustache” is a row of ultrasound transducers that push sound waves into the blood vessels and capture the returning sound waves. Those returning signals measure blood pressure and heart rate.
The sensor is capable of measuring three parameters at the same time, one from each sensor. For example, simultaneous readings of blood pressure, glucose and lactate levels, alcohol or caffeine. The laboratory is working on a more advanced design that would allow all parameters to be monitored simultaneously.
The patch has the potential to improve healthcare monitoring in a wide range of situations. “It could serve as a great tool for remote patient monitoring,” explained Sheng Xu, PhD, assistant professor of nanoengineering, bioengineering, and electrical and computer engineering at UCSD and co-senior author of the study, “especially during the COVID-19 pandemic, when people minimize in-person clinic visits.”
The technology would benefit people with self-managed underlying conditions, such as hypertension and diabetes. It could also be a game-changer in more critical situations when placed on the neck or forearm of patients in intensive care units, including babies in the NICU, who need continuous monitoring of blood pressure and other vital signs, measures currently accomplished by invasively strapping patients to an armada of inelegant, expensive and often noisy hospital monitors.
The new sensor patch was developed by overcoming a number of engineering obstacles. For example, ultrasound transducers typically require a liquid gel to send and receive signals. But that gel would interfere with nearby chemical sensors in the small patch. The engineering solution was to develop a solid gel that worked with ultrasound but could not flow or block the function of adjacent chemical sensors.
In fact, the patch’s engineering requirements required collaboration between two UC San Diego research groups. Sheng Xu’s lab has pioneered work on electronic skin patches that are soft and can stretch with the skin and can monitor blood pressure. The laboratory of Joseph Wang, PhD., specializes in the development of wearable devices that can monitor multiple signals simultaneously: chemical, physical, and electrophysiological. Wang is president of SAIC and a distinguished professor in the Department of Nanoengineering at UCSD.
“The collaboration of our two laboratories has been absolutely essential to the development of this technology,” Wang explained. “And this is just the beginning. Our combined experience will allow us to pursue sensors that can collect even more information using this convenient, non-invasive style of patch. Additionally, the current patch is still physically connected to a receiver. We are now working to add the receiver to the patch, which means no more wires. The patch will send signals remotely, allowing for extremely convenient continuous health monitoring in virtually any environment.”
This research was supported by the UCSD Wearable Sensors Center and grant no. 1R21EB027303-01A1, CNPq, a UC MEXUS-CONACYT Collaborative Scholarship, the Fulbright Egypt Scholar Program, and the Royal Golden Jubilee PhD Scholarship from the Thailand Research Fund. The work was published in Nature Biomedical Engineering.1